We answer the questions do I need to gain weight and go all in to get pregnant and get back my period with hypothalamic amenorrhea (HA) and how does it differ from PCOS?
Having children is a lifelong dream for many people. It’s something some of us have dreamt of since we were children ourselves. Unfortunately for some of us, by the time we actually want to get pregnant, we realize it’s not as simple as having unprotected sex. In fact, a full-term pregnancy can seem like an actual miracle.
Infertility is a heartbreaking struggle that many people experience. In fact, 1 in 6 couples have difficulty getting pregnant. While there is no official definition of infertility, it’s commonly defined as the inability to conceive after a reasonable period of unprotected sex. For women under 35, this is about a year of trying and for women over 35, it’s about 6 months.
There are several reasons for infertility and both women AND men can experience it (sometimes both partners at the same time.)
Unfortunately, women’s fertility begins to decline in their mid-30’s (although this is very individual!) So, simply being older is a common reason why women struggle to get pregnant. Previous STIs, hormone imbalances, endometriosis, uterine polyps or fibroids, blocked fallopian tubes, and menstruation difficulties are other common causes of infertility.
Why your Period is Important to Getting Pregnant
Although we sometimes wish didn’t get our period, it’s actually a very important indication of health.
A female menstrual cycle lasts between 28-30 days and involves a variety of important reproductive hormones. To be brief, the hypothalamus in our brain releases a hormone called Gonadotropin-releasing hormone (GnRH) which works on another part of our brain called the pituitary gland. This causes a release of two hormones called luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Together, LH and FSH act on our ovaries to release estrogen and progesterone, which allow for our uterus to prepare for pregnancy by creating a thick sticky lining. Around week 4 of the cycle and no sperm in sight, this lining begins to shed and is what we know as our period.
If there are irregularities or no period at all (known as amenorrhea), then this can be a sign of a health problem.
Amenorrhea is defined as the lack of a menstrual cycle for 3 or more months in women that have previously had menstrual cycles. While birth control and genetics may play a role in amenorrhea, the most common causes of amenorrhea include polycystic ovarian syndrome (PCOS) and hypothalamic amenorrhea (HA).
For more information on hypothalamic amenorrhea, I highly recommend this book: No Period, Now What?
Here’s the problem: these two very different conditions are often misdiagnosed for one another, yet the treatment and recommendations are completely opposite. If you’ve lost your period and are wondering if you need to gain weight to get pregnant or perhaps lose weight to get pregnant, you’ll want to get a clear understanding of the differences between HA and PCOS. In this post we break it down.
What is PCOS? Who’s at risk?
PCOS is one of the most common endocrine disorders in pre-menopausal women and affects a whopping 1.4 million Canadian women or about 12% to 18% of the female population.
Unfortunately, researchers aren’t sure why women develop PCOS, but it has three main features and you must have at least two to be diagnosed:
- High levels of androgen (male) hormones such as testosterone
- Irregular or missing periods
- Numerous cysts in the ovaries (“polycystic” translates to “many cysts”), usually diagnosed as 25 or more cysts.
Insulin resistance and genetics appear to play a role in PCOS. When insulin levels are high, this can lead to an increased production of male hormones. While many believe that weight loss helps with PCOS, it often ignores the risk of disordered eating and weight cycling that follows. Instead, focus should be on healthy eating habits that are designed to fuel your body, rather than depriving it. This may include working with a dietitian to review how your body responds to certain foods.
Usually women who present with PCOS have lower female hormones, such as luteinizing hormone (LH) and follicle-stimulating hormone (FSH), and higher levels of male hormones. This leads to a disruption in ovulation and can prevent a complete menstrual cycle from happening.
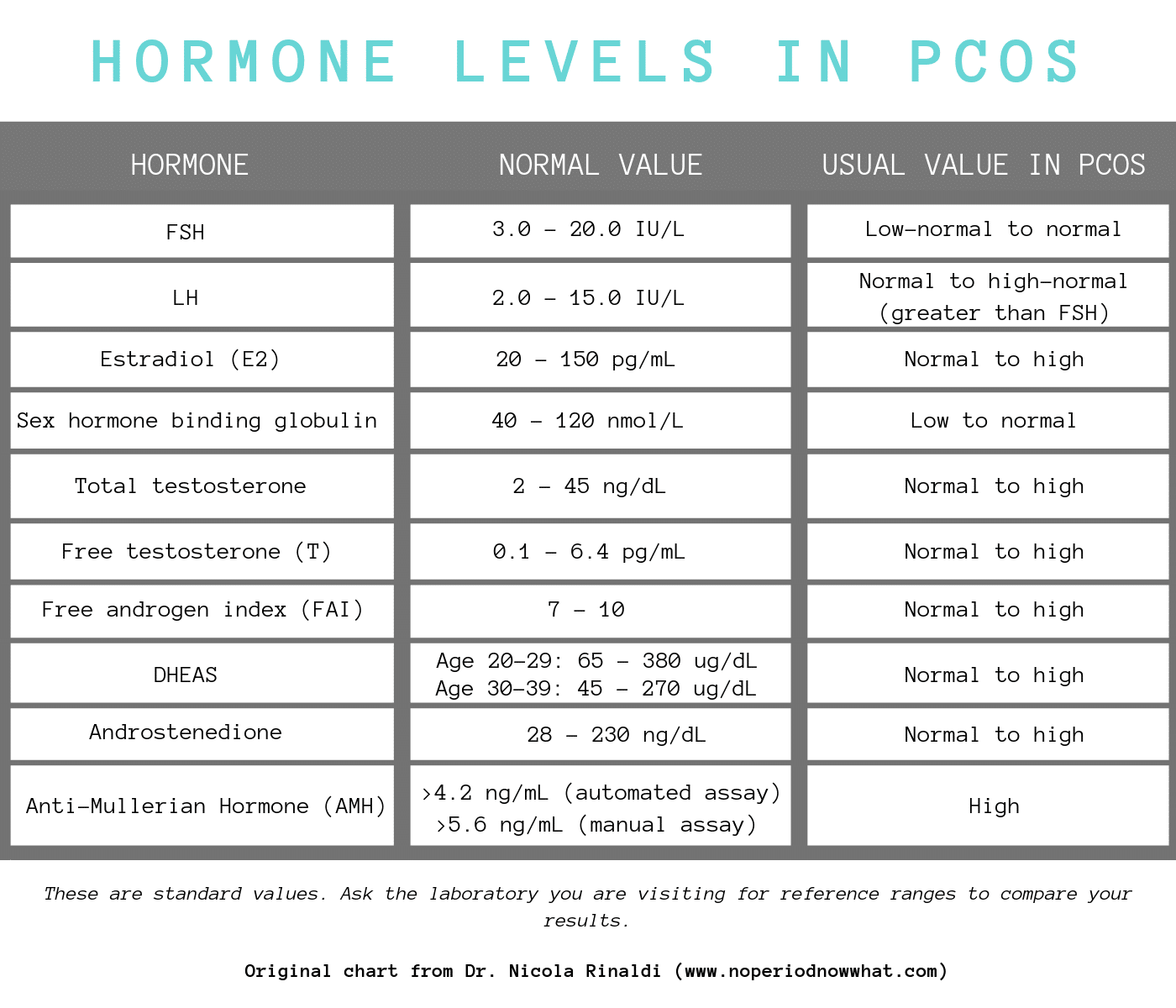
In the chart below, you can see how women with PCOS have altered hormone levels.
- Weight gain, especially around stomach
- Higher body weight – over 50% of women diagnosed with PCOS have a BMI over 30
- Insulin resistance
- Excess hair in uncommon areas such as the face, chest, abdomen, and back
- Hair loss on scalp
- Acne
- Dark patches of skin in body creases (e.g., groin, neck, under breasts)
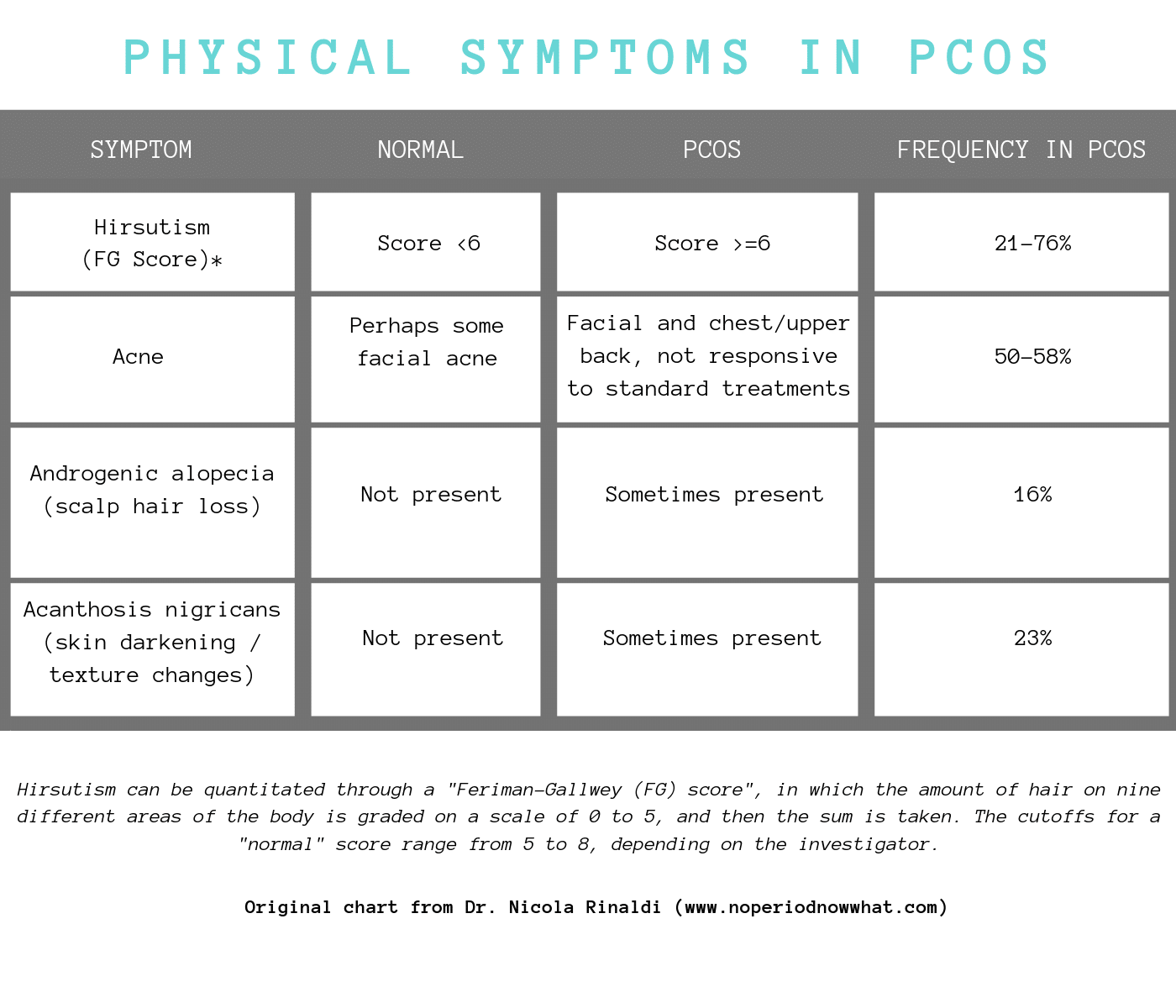
When it comes to physical symptoms (see below), it can vary from person to person.
What is Hypothalamic Amenorrhea (HA)? Who’s at risk?
Hypothalamic amenorrhea (HA) is defined as loss normal menstruation for 3 months or longer and is usually due to low calorie intake, excessive exercise, psychological stress, genetic predisposition, or a combination.
Remember earlier when I mentioned our menstrual cycle heavily relies on the hypothalamus? Well, that’s why this condition is called hypothalamic amenorrhea! Since it describes the symptom (aka no period) and the reason for it (the hypothalamus).
While both HA and PCOS can result in loss of period, the main difference is that HA is usually related to lifestyle influences, while PCOS is an endocrine disorder.
HA affects approximately 1.62 million women in the US or about 17.4 million women worldwide, although it’s likely much higher in women who participate in sports that require leanness, such as ballet, figure skating, and physique competitions (or bodybuilding).
The main driver of HA is a large energy deficiency, which comes either from extreme exercise, undereating, or both. This also means that ANY woman can experience HA, regardless of their body size since we all have our own unique set points. In other words, you don’t have to look like a fitness model to lose your period and have a difficult time getting pregnant.
According to an expert review in The Journal of Clinical Endocrinology and Metabolism, decreasing daily calories by 470 – 810 calories (or less than 30 calories per kilogram body weight per day) has been linked to a higher risk of HA. This paired with excessive high intensity exercise places you at an even greater risk.
Psychological stress can also lead to HA. In fact, research has shown that women with HA tend to have “”perfectionist” tendencies. Our body’s menstrual cycle is heavily influenced by stress. Stress can be psychological, such as ongoing stress at work, home, in our relationships, and so on. Stress can also be physical, meaning over-exercising or not providing enough calories can cause significant stress on the body. This stress heavily influences activity of the HPA axis (aka. hypothalamic-pituitary-adrenal axis) which is one of our main stress response systems.
Ongoing stress causes the body to release high levels of cortisol, a stress hormone which decreases levels of GnRH (Gonadotropin-releasing hormone), which if you remember is responsible for LH and FSH.
When these levels are low, we may lose our period and as a result, may have a difficult time ovulating and getting pregnant.
Common signs of HA include:
- Amenorrhea (lack of period)
- Digestive problems
- Impaired immune system
- Brittle hair & nails
- Always cold
- Extreme hunger
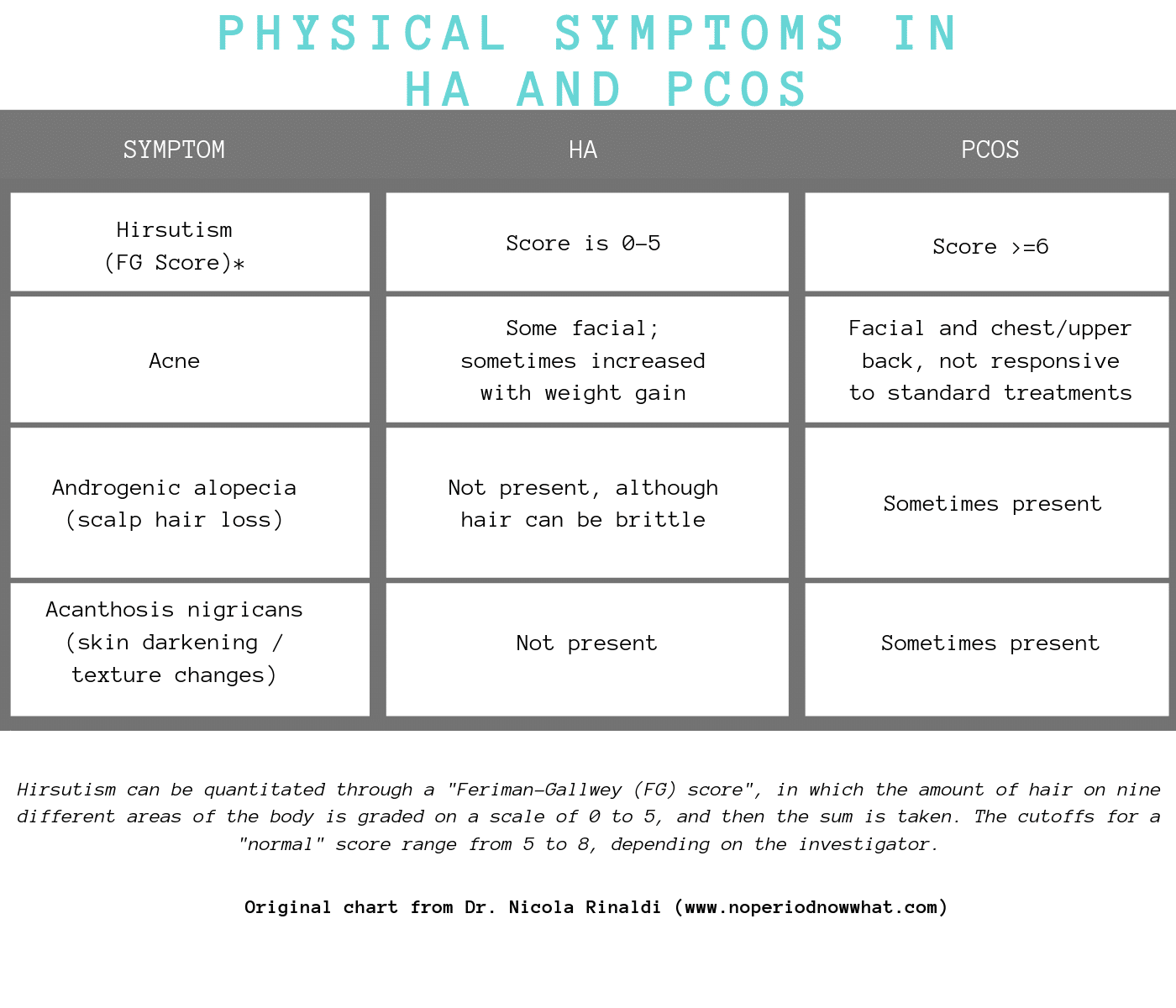
When it comes to HA, women do not present with the same physical symptoms as women with PCOS. This is outlined in the chart below:
HA is usually a diagnosis of exclusion, meaning your doctor will rule out other disorders first, such as thyroid issues, PCOS, and ovarian insufficiency. Usually, HA is defined as lack of a period for at least 3 months and low female reproductive hormones, usually accompanied with extreme energy restriction.
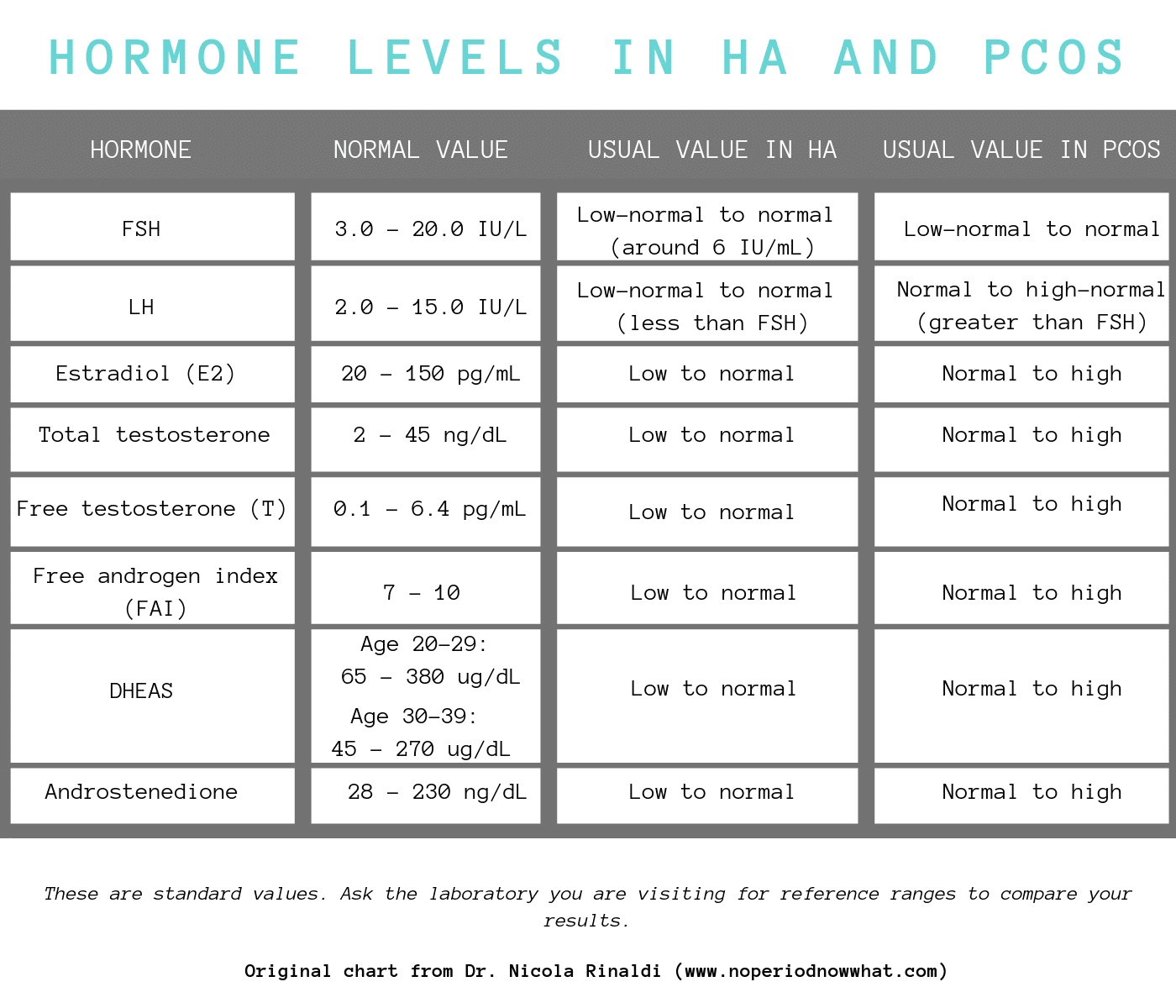
Again, women with HA have different hormone levels than women with PCOS, which is outline in the chart below.
How does treatment differ for HA and PCOS?
When it comes to HA and PCOS, treatment is VERY different, which means it is crucial that you get a proper diagnosis.
For PCOS, especially in women who have a high BMI, weight loss is usually recommended along with medications to normalize your estrogen levels, stimulate your ovaries, and/or improve insulin levels (like metformin). This means that your doctor may recommend eating fewer calories and exercising more. However, diets usually lead to a cycle of weight loss and weight gain, which can make PCOS symptoms even worse. Fortunately, lifestyle changes such as moderate exercise and intuitive eating can be effective in managing PCOS and doesn’t require you to fall victim to diet culture. You’re better off focusing on foods that fuel and satisfy you, which can still keep insulin levels in check without depriving yourself.
Unlike with PCOS where I feel that purposeful weight loss below one’s set point should not be the goal, with HA weight gain is often necessary. This is done through increasing calories and decreasing exercise frequency and/or intensity. This can be very scary for most women, since our society unfortunately paints weight gain as the worst thing that could happen to us (reality check: it’s not!)
Do I Need to Gain Weight to Get Pregnant with HA?
According to Dr. Nicola Rinaldi, leading expert in HA, very likely yes. If the goal is to get a period and get pregnant, many experts recommend drastically increasing caloric intake to wake your hypothalamus into action, a method sometimes referred to as going “All In”.
How do I Go All In to Gain Weight with HA?
Now, before you think this idea is crazy and overwhelmingly scary, too much so to even entertain, hear us out. There is real evidence behind going all in to gain weight to get pregnant.
During periods of calorie restriction, the body tries to protect itself from starvation by slowing its metabolic rate so that it burns fewer calories. So, for women with HA, they’re likely metabolically inefficient. This means that their body requires more calories than normal to restore body weight and maintain regular body function. Considering most women need somewhere around 2,000 calories per day, a person with HA will need to eat well over this to restore their metabolism just back to baseline, so most experts recommend somewhere between 2500-5000 calories.
By gaining weight, you are taking your body out of metabolic stress, which allows hormone levels to normalize and resume a regular period. In fact, many doctors state that a BMI of 20-24 is the “fertility zone” and increases your likelihood of getting pregnant. This means that if your BMI is 19 or lower, you may have difficulty conceiving a child.
Decreasing exercise intensity and frequency is also crucial to HA recovery. The body needs to be in an energy surplus to gain weight, which is difficult if you’re still exercising at high levels. Furthermore, we want to decrease the level of stress on the body. Since exercise is a type of stress, this doesn’t give the body enough of a chance to recover properly. I know for a lot of us we think that exercise is actually a stress reliever- and it can be! But when your body is under metabolic stress, as is the case with HA, the impact exercise has on cortisol is counterproductive to recovery.
Finally, treatment usually involves working with a team of trained professionals who specialize in disordered eating. In addition to diet and exercise, many people also undergo Cognitive Behavioural Therapy to help identify positive coping strategies to replace unhealthy and harmful behaviours.
Extreme Hunger, HA and Going All In
When our bodies are deprived of calories for a long period of time and we experience extreme weight loss, it goes into survival mode. One of the most common survival mechanisms is extreme hunger. Basically, the body begins to release high levels of ghrelin, a hormone that tells us that we are hungry. Very VERY hungry. At the same time, it decreases levels of leptin, a hormone that suppresses our appetite. This can lead to extreme hunger even if we begin to eat more calories. Since HA causes our metabolism to become inefficient, many people require high volumes of food to satisfy their hunger and ultimately, gain weight.
While many body competitors with HA try to reverse diet, which involves slowly increasing calories over weeks to return to a normal weight, it doesn’t address extreme hunger. As a result, many women have turned to going “All In”.
Going “All in” involves eating a high number of calories each day (sometimes upwards of 5,000 calories) to gain weight and restore one’s metabolism back to normal while also resolving extreme hunger. This may involve reaching an “overshoot” weight, which means gaining more weight than the person’s natural set point. To be brief, set-point theory suggests that the body works to maintain a predetermined weight through regulation of metabolism. Essentially, the body will slow the metabolism when underfed and increase metabolism when overfed to minimize large changes in one’s weight.
People that go “All in” will continue to eat this way until their weight gain plateaus. At this point, you may start to feel more satisfied on fewer calories and potentially may lose a bit of “overshoot” weight as your body settles into its natural set point. This overshoot weight may or may not happen, so I recommend not going into the process of All In for fertility thinking that you will lose the weight you gained. You MAY lose some, but likely if you found yourself with HA, you likely were well below your natural set point weight.
What Can I Expect to Happen with my Weight when I Go all In?
Every person will have a different experience when going “All in” because we all have different bodies and different set points.
As mentioned, going “All in” involves eating a high number of calories to restore your metabolism and resolve your extreme hunger. Although 5,000 calories sounds like A LOT, you may not need this much to feel satisfied. This is just a ballpark and Dr. Rinaldi recommends 2500 as a MIMIMUM with no maximum. The goal of going “All in” is to eat to fullness, which is a stepping stone to retraining yourself to eat intuitively. Instead of worrying about a certain number of calories, you simply eat until your body tells you you’re done.
When recovering from HA, your body may ask for more calories than what you may perceive as “normal” in order to help you return to a healthy weight and kick start that metabolically inefficient hypothalamus. You may gain weight quickly or slowly, but your body will naturally direct you to what it views as a healthy weight for you.
Does Going All In Mean I Have to Eat 5000 calories a Day Forever to Cure my HA?
No, you won’t! You may need to eat a lot of calories for a while until your metabolism and hunger are back to normal, but after a while, your body won’t require as many calories to feel full and you can slowly return to eating a regular diet.
The Bottom Line on Gaining Weight to Get Pregnant and Get Your Period Back with HA
Infertility is devastating to a family looking to grow. In many cases, your doctor can help find solutions to improve your chances of conceiving, some of which may include treating your PCOS or HA.
PCOS and HA are both treatable conditions that can usually lead to pregnancy if managed properly. However, it is important to visit your doctor to ensure you have a proper diagnosis because, as we have talked about, treatment is VERY different. It’s also important to openly and honestly communicate with your doctor about your lifestyle habits to make sure they have the whole picture. If your doctor isn’t listening to your concerns (which unfortunately is the case for women’s health too often) then it may be best to find a new doctor.
As for the idea of gaining weight to get pregnant and get your period back, I get that this may be an anxiety provoking thought – especially if your diet or exercise regime are a big part of your identity and life. As a society, we have been spoon-fed the idea that having body fat is bad. Yet, research continues to tell us that body fat is a natural and crucial part of overall health, especially reproductive health. Of course, the diet industry can’t make money on this and will continue to do anything to convince us of the opposite.
I encourage you to take a minute to evaluate your priorities. Do you really want to spend your life striving to reach an unattainable and unstainable standard of beauty that puts your health and family in jeopardy? Diet culture says yes, but we need to say no. While pregnancy is the goal for many of you, I want you to think long-term. Changing your values towards long-term metabolic health will not only help you get pregnant, but will ensure you live a long, energized, happy life to enjoy that child with, too.
Now tell me, do you or someone you know suffer from HA or PCOS that is impacting your fertility and ability to get pregnant?
Have you found that gaining weight has helped you get pregnant?
Leave me a comment below!
Contribution by Katey Davidson, RD of a Taste of Nutrition
Updated on July 24th, 2020

Abbey Sharp is a Registered Dietitian (RD), regulated by the Ontario College of Dietitians. She is a mom, YouTuber, Blogger, award winning cookbook author, media coach specializing in food and nutrition influencers, and a frequent contributor to national publications like Healthline and on national broadcast TV shows.











jafeth says
I am trying to regain my period after a year of bodybuilding prep… I am 4’11, do i still need 2,500 calories per day minimum? I want to make sure I am doing “All IN” the right way.
Abbey Sharp says
That is the standard recommendation for all in but I can’t speak to wether or not the recommendation would be less for your case. If you need more detailed information on this topic I would highly recommend Dr. Rinaldi’s book “No Period. Now What?”
samantha says
I have HA and I’ve finally decided to eat at least 2500 calories a day and cut out high intensity workouts (I only do pilates, stretching, strength training, walking for 4 times a week). I know a lot of people with HA have extreme hunger but I actually have no hunger at all (and I don’t have any fullness cues. I can eat a full meal and feel the same as before). do you know possibly why I might not have any hunger or fullness? im so confused…do you think that it has to do with the hormones having to do with the hypothalamus and once I get my period back, ill have the cues? sorry for all the questions.
Abbey Sharp says
Its not uncommon when you’ve been undereating for a long time to lose hunger cues. This is because your body has relegated energy to other things (like surviving) since the cues have been ignored for so long. once you start fueling your body regularly and it starts to trust that food is coming, those cues will return.
Nicole says
This has a lot of really helpful information, so thank you. You mention a chart that breaks down all the info a few times in the article, but I couldn’t find it. Now, this may be a total face-palm moment on my part, but is there a chart that I’m missing?
Abbey Sharp says
Hi Nicole. Thank you for flagging this! We’ve added the corresponding charts to the blog post. I hope thats helpful 🙂
Liz says
I think it’s worth adding that a lot of women with HA get misdiagnosed with PCOS. With HA, you can sometimes end up with a lot of follicles that never quite make it, leaving ovaries that do appear to be polycystic on an ultrasound. I think any history of disordered eating or under-fueling or over-exercise, even at a healthy BMI, and especially absent high androgen levels, should be assumed to be HA. I’m only saying this because I have been misdiagnosed many times, as have a lot of women I know with HA. It is possible to have both, but it’s not common.
nina says
is it possible to recover from HA just by eating a lot more without stop exercising?
Abbey Sharp says
its definitely possible, it’s all about making sure your fat stores are in a good shape and youre not burning too many calories vs eating. so it may slow your progress but not impossible.
Julia E Weiland says
I liked the article but I did not love that you referred to testosterone as a “male” hormone. It adds to the misinformation about PCOS. Both women and men have testosterone in their body, PCOS is just associated with higher than normal levels. Many women feel unfeminine when having PCOS due to the issues with body hair and fertility and I don’t think the way you phrased this is helpful.
Abbey Sharp says
hey Julia, thanks for your feedback.
Nina says
Hi! Thank you for this article.
I had amenorrhoea for 6 years when I was underweight. I reached a set point when i started to recover from my eating disorder. During my exams, which was a stressful time, I again lost my period; I now haven’t had it for about 6 months.
I don’t know whether that is HA or not- I can’t stop when I start to eat and I then go through mental restriction which makes me eat MORE than intended- does this mean I have Binge Eating Disorder?
I am really confused. I am in the healthy weight range at the moment. If I do have HA, how come I am not underweight? Even at my “plateu” or (what I am pretty sure is my) set point, I was around the same weight. My main question is: Why am I eating so much and don’t have periods?
– eating too much because mental restriction
– no periods because of stress (but not related to food)
What should i do?
Nina says
edit:
I lost my period for 6 years in 2009 (very low BMI), then got it back in 2016 (healthy weight, set point), then lost it again 6 months ago (similar weight, maybe 1-2 kg less, but nothing extravagant and unintentionally). What is going on?! Currently I am set point + a little more (I think. I did not weigh myself)
Do I eat more or less? I don’t want to gain an unhealthy amount of weight. I want to get rid of the cravings and I think by letting myself eat ANYTHING, I will get over this. OR if I let myself eat everything, I will get addicted to “junk” and continue to gain weight. I have already started gaining weight now.
What do I do?
Nikki says
I have had HA for 6 years. I have reduced my exercise and gained 6kg from a starting weight that was low but not considered underweight. I just cannot get my period back! I’ve never had an eating disorder. I’ve also tried increasing carbs, taking bio identical (not synthetic) progesterone and acupuncture. Is there anything else you can suggest? Nothing is working.
Abbey Sharp says
Hi Nina, I recommend meeting with a dietitian. They can provide some recommendations to meet your needs.
Mariam says
Hello, Abbey.
I have read your important and informative article. I am 32 years old and unfortunately I am suffering from HA.
Since about 2 years I have begun to follow a “healthy diet/lifestyle” which focuses on wholewheat and plant-based food; I am not a vegetarian or vegan.
I was okay during the first year but recently I experienced weight loss, lack of energy – I know that I have restricted my calories. I have to admit that.
The problem now is that I badly want to restore my period without depending on unhealthy food, so I want you to talk about, “How we can gain weight healthily?”, because I don’t want to gain weight by eating junk food or foods that contains high levels of sugar as it can have a serious effect on my health.
Thanks in advance.
Abbey Sharp says
Hi Mariam, I recommend meeting with a dietitian to discuss healthy weight gain.
Aleksandra says
This is the most terrifying article I have read in my life, because every.single.word is about me.
I am suffering from PCOS (confirmed by an ultrasound & lab works), but I am also well below my natural healthy weight, with a BMI of 18.4. I have disordered eating habits, I count calories, restrict, punish myself and feel shitty about eating. Yeah, the entire package. And I haven’t had a natural period in a year (only couple of times when doctor put me on progesterone, that worked) and now I wonder, which one is it – PCOS or HA. I pray it’s PCOS because there is no way in hell I could go with all in. I would proabably end up depressed and on xanax, because eating gives me anxiety. I eat enough not to starve myself and I do reward myself with a bottle of wine or a pizza during weekends, but that’s about it. I’ve been doing it a while and I know it doesn’t affect my weight, so I have my limits of indulgence. But an unexpected office party with free cake? No way, there’s no room for that, did not plan ahead for such event.
Long story short, my husband and I were thinking about kids (hence discovering I have PCOS), but I do not think it will ever be possible…
Thank you Abbey for that post!!! I will save it. For some better time.
Abbey Sharp says
Hi Aleksandra
Thanks for your honest message. So there are tests for PCOS so you can rule that out but based on your description I would put money on this being HA. The good news is HA is way easier to manage then PCOS, so this would actually be a good thing. The fact that you wish so much to have an incurable disease vs a very easy to manage via weight gain one indicates there may be a disorderly unhealthy mindset going on and I strongly suggest seeking some counselling from a RD who specializes in eating disorders. I really wish you the best on your fertility journey.
Mae says
I never knew HA existed before! Can you have HA, or all the symptoms of it including the hunger and the high cortisol, without the actual amenorrea?
Abbey Sharp says
I don’t believe it would officially be classified as HA, but it may be treated the same (ie weight gain)
S says
I have HA and have found it hard to find a dietician or doctor who agrees with the “all in” mentality. I’ve seen three dieticians and a reproductive endocrinologist who all think it is too extreme since I’m a “normal” weight. Your post is refreshing and makes me feel a little less crazy about going all in. I think there are a lot more girls than we realize who struggle with this, and I hope they find this post. Thank you!
Abbey Sharp says
Even though you’re a “normal” weight, you might not be at your body’s optimal fertile weight. I’m sorry for your experience!
Caitlin Mackay says
Hi Abbey! love your post.
I find myself currently battling with potential HA. However, I have never truly had a regular menstural cycle and I’m only 18.
I worry that i’ll never have a normal cycle as I’ve transitioned from 16 stone to 9 stone in 3 years, but I’ve never had a normal cycle during my steady weight loss period.
I have undergone blood tests and ultrasounds and have been told that my hormones and reproductive organs look fine, So from process of elimination, I am assuming that my lack of period is down to calorie restriction.
I now find myself wanting to live a life where I am no longer as food obsessed and trapped in toxic diet culture, and want to eat foods that fuel the training I do, as I have always loved being active!
I would love to get in touch for some healthy meal recommendations, full of vitamins, minerals and energy to fuel my future and maybe even possibly have a regular cycle!
Thank you kindly!
Abbey Sharp says
Hi Caitlin. Thanks so much for sharing. I recommend meeting with a Dietitian who can provide you with those healthy meal recommendations to meet your unique needs.
Lorie says
A very interesting g and resourceful article, Abbey. With our own infertility I wish we had answers—periods were regular so there never seemed to be much an issue ??♀️
Abbey Sharp says
For sure. Thanks Lorie
Stephanie McKercher says
This post will help so many people, Abbey! I honestly didn’t know infertility is so common. 1 in 6 seems like so many people! Glad we are talking about this topic more.
Abbey Sharp says
For sure. Thanks love
Angela says
This is a very thorough and well researched post on HA. I have to admit I did not know much about it before reading this, very interesting!
Abbey Sharp says
Thanks for reading Angela