We explore the long-term outcome of excessive sanitation products in the Covid outbreak, and answer the question are disinfectant wipes, Lysol, bleach, and hand sanitizer safe for our health and microbiome – particularly for children or pregnant women?
As you’re likely aware, unless you’ve been sleeping through 2020 so far, there is a worldwide shortage of sanitizing products available for purchase at just about every store in North America. This is because of one simple thing: everyone under the sun is now purchasing them at a MUCH faster pace and using them in a greater abundance than they likely ever were before. People are not only constantly wiping off door handles and sanitizing their hands after putting gas in their car, but they’re also wiping down every grocery item or delivery that comes to their door. I have even heard of people washing their produce in bleach! (SIDE NOTE: DO NOT DO THAT. I have a whole post on how to safely sanitize groceries and take-out right here) and it doesn’t have to be THAT extreme.
I want to reiterate that, of course, keeping you and your home clean with regular hand washing and other hygienic practices is absolutely essential to fighting Covid-19 and other viruses, but a lot of people have been questioning the potential risks of this hypervigilant state of sanitation.
Why would we ever worry about being too clean, you might ask? Because there has been a long-standing theory in the world of germs, the microbiome, and health, which posits that a state of over-sanitation early in life (aka during childhood) may actually be linked to poorer health outcomes due to a diminished exposure to the germs that actually help to maximize our immune system. This theory is known as the “hygiene hypothesis”, and while there is tons of speculation and controversy surrounding this hypothesis and its validity, the trend still remains that as we became an industrialized nation, and sanitation practices were heightened, so too did the incidence rates of allergies and autoimmune diseases like type 1 diabetes, asthma, Chron’s disease, multiple sclerosis, and inflammatory bowel disease.
BUT as we preach here at Abbey’s Kitchen, correlation doesn’t always equal causation. So, to get a clearer picture of if there really is any cause for concern with the COVID-19 induced over-sanitation trend, I took a deep dive into the research surrounding the hygiene hypothesis, sanitation practices, and our microbiome!
The Hygiene Hypothesis
First, let’s chat about the hygiene hypothesis and how it came to be. The hygiene hypothesis was first developed in the late 1980s by an epidemiologist, Dr. Strachan. He found that there was a relationship between an increased family size (i.e. more children) and a reduction in the development of autoimmune diseases and allergies. He proposed that the decreased incidence of infection early in life, typically passed through “unhygienic” contact between siblings, could be the cause of developing autoimmune complications later in life. Following this hypothesis, much more research took place surrounding this phenomenon, and the belief shifted towards the notion that a decreased exposure to microbes in early years is a major risk factor for developing autoimmune diseases later in life. Even at this time, it was noted that there was a wide range of factors at play when it came to a diminished microbial exposure, including “clean water and food, sanitation, antibiotics and vaccines, birth practices, as well as incidental factors such as the move from farm to urban living”. However, for many people, the concern narrowed in on sanitation practices. Because of this, there has been recent controversy over the hygiene hypothesis, and the misconceptions that were developed because of it.
Many scientists attest to the name and wish to see it changed, seeing as the term “hygiene” is often misinterpreted as being synonymous with personal cleanliness like hand washing, cleaning foods, and washing soiled floors and counters. However, that should not be the case – these personal sanitation practices are one of our first lines of defense against harmful bacteria, therefore, ceasing to take part in them would put us in harm’s way. The concern instead is when these “sanitation practices” are taken to an extreme or directed at situations that are not actually harmful, significantly limiting children’s healthy exposure to the microbes (that is, bacteria) in their environment. Many of the researchers who wish to see the name of this theory changed have offered up alternative names, such as the “microbiome depletion hypothesis” or the “microbial diversity hypothesis” – no such luck so far though (guess it doesn’t have the same ring). But, names aside, the foundation on which this hypothesis is based on still does hold some merit according to recent research. More recent research has taken the foundation on which the hygiene hypothesis was laid on, and developed clearer guidelines and recommendations surrounding sanitation and hygiene. The most supported approach for ensuring safety as well as health in the home is targeted hygiene.
Targeted Hygiene
The hygiene hypothesis is reportedly pinpointed on home sanitation as the root cause of adverse health outcomes, which is where it falls short. Instead of focussing solely on over-sanitation being responsible for the rise in allergies and autoimmune diseases, we must look at the bigger picture and recognize that it is likely much more complicated than that. Evidence now suggests that a combination of strategies should be integrated into young children’s lives in order to best protect their microbiomes from complications later in life. These strategies include vaginal childbirth (if possible), breast feeding (if possible), increasing social exposure through things like sports, social interactions, and outdoor activities, having pets like cats or dogs in the home, as well as appropriate antibiotic use (aka only using them when it is absolutely called for as of course, these save lives). Another way of looking at this is through “targeted hygiene” – where risky activities, like touching raw meat or using the washroom, should be followed with proper hygienic practices, but at the same time, playing outside in the soil, petting the family dog and sharing toys with peers should be encouraged. Targeted hygiene allows for the protection against harmful pathogens, while also promoting and allowing for the healthy spread of microbes between peers, family members, and the environment. Allowing for the introduction of such microbes is important for the establishment of a healthy immune system, which, for the most part, is trained by the age of 4. This keeps our immune system in balance, protecting it from overreacting to non-harmful particles – which is the underlying mechanism of allergies.
Can we improve our microbiome later in life?
Not to fret if you’re already 5 or older! While the microbiome may be largely shaped during the early years of life, the colonies within the gut microbiota are still largely unstable during childhood and become more stable during adulthood. This means that the commensal bacteria which colonize our microbiomes become more balanced and stable within the later years of life. There are also strategies that can be utilized in youth and adulthood in order to develop a robust microbiome, including consuming a sufficient amount of fruits and vegetables, whole grains, and exercise. Recent research links the Mediterranean diet, a diet rich in whole foods, grains, and healthy fats, to a significant increase in beneficial microbes in our gut. Therefore, if you are at all concerned about your microbiome, transitioning to a more balanced and whole-food diet may be a good place to start.
While, undoubtedly, more research is needed in this field, there have ALSO been several strong connections made to those people with the lowest incidence of allergies and their relationship with microbes. First, early-life exposure to siblings is correlated with a lower likelihood of allergies – this is thought to be connected to microbes being passed between siblings through “unhygienic” contact. Second, having pets (i.e. cats and dogs) in the house can help to develop a stronger immune system, even before birth while a child is still in utero. This is because people can share their microbiota via contact with dogs, meaning having them in the house can greatly increase the microbial biodiversity. Other research supports the fact that early exposure to our natural environment is crucial for developing a well-rounded immune system and microbiome. They have found that exposure to farm environments within the first 2-3 years of life can be protectant against developing allergies, while other studies show that even living close to agriculture or green space can protectively increase the biodiversity of our microbiota.
Bottom Line on Hygiene and our Microbiome
Healthy exposure to safe microbes from our environment and each other is NOT a bad thing, in fact, it is a very good thing. HOWEVER, let me reiterate, these studies are referring to the beneficial (or, at the very least, not pathogenic) microbes found in our environments – so, I am not saying to stop cleaning your house and sanitizing in an effort to avoid being infected with COVID! That would be ill-advised and is one of the main qualms that scientists have with the name and premise behind the “hygiene hypothesis”. What I am saying is this: being able to recognize low-risk situations and not overreacting with sanitation protocols may be beneficial for our children’s health later in life.
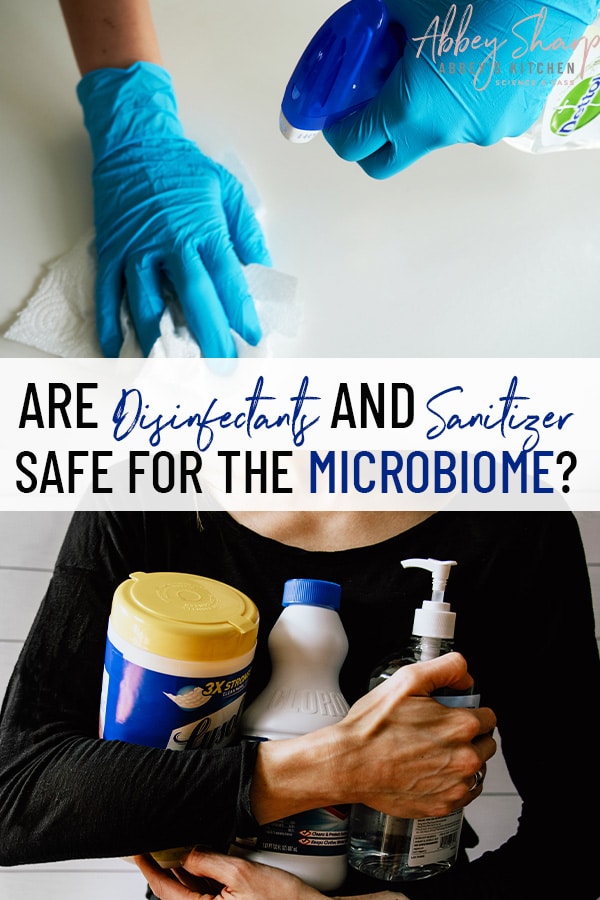
Are Using Excess Disinfectant Wipes, Lysol, Bleach, and Hand Sanitizer Bad for our Microbiome?
While the evidence here is very preliminary and done primarily with animals that are fed a diet with these chemicals in it, there is early evidence suggesting that when/if antimicrobials enter into our body, if not handled properly, it may affect our microbiomes. Much of the research studies focus on compounds called triclosan and triclocarban. Triclosan is an antimicrobial agent that is added into a lot of household cleaning supplies, as well as soaps, toothpaste, and some cosmetics. The FDA is continuing to monitor this chemical, and is aware of the studies being done to test its safety for human use. They also did ban the use of both of these chemicals in consumer soaps in 2016, indicating they recognized a safety concern with over-exposing oneself to them. One study found that zebrafish which were fed a diet containing triclosan experienced an alteration in their gut microbiota after only 4 days. Another study, which focussed on humans, found an altered gut flora in children who were frequently exposed to household disinfectants. These children were then linked to having a higher body weight by the time they were 3 years old when compared to the children who were not exposed to heavy home use of disinfectants. This is just correlation, and what we don’t know is if the families who chose “greener” methods of cleaning ate “healthier”, were of higher socioeconomic status, were more likely to be breastfed or had more access to the outdoors, attributing to a different outcomes in their microbiome and weight. Another thing to note is that while this study did find a difference in the microbial community composition of the children who were exposed to non-eco-friendly chemical products, they did not find any changes in the microbial richness or diversity. This means, essentially, that there were more microbes introduced which were linked to weight gain and/or negative effects, but there was no negative impact on the already existing microbial community – that is the number or type of pre-existing microbes.
Bottom line, the research in this area isn’t great period and we need a lot more of it. But the good news is that of ALL the links between hygiene and the microbiome, researchers believe that “being too clean in our own homes” is one of the weakest and most un-supported notions perpetuated by the “hygiene hypothesis”. It is believed that if over-sanitizing the home contributed to an increased risk of allergies or autoimmune diseases, it would be a relatively small contribution. This is because microbiological studies have confirmed that regular cleaning habits, while decreasing pathogens and dust temporarily, do not have a sustained effect on microbes in the home. One review article claims that “the idea that we could create ‘sterile’ homes through excessive cleanliness is implausible; as fast as microbes are removed, they are replaced, via dust and air from the outdoor environment, and commensal microbes shed from the human body and our pets, and contaminated foods brought into the homes”.
Are Sanitizers and Disinfectants Safe to Breathe In?
Many online sources point towards household cleaners are being dangerous for our overall health, claiming their detrimental effects on our lungs. While more research is most definitely needed to support these claims, especially when it comes to humans, there have been some preliminary studies trying to address these claims. One study, accomplished through the European Community Respiratory Health Survey, found that people who worked as cleaners or frequently cleaned their homes with chemicals had decreasing rates of lung function. This finding was only true for women and was more apparent the more time the women spent around chemical cleaners, notably those which were sprays or were aerosols. This indicates that there may be a link between frequent cleaning activities and respiratory health (which is concerning in a global pandemic surrounding respiratory health). Other studies have linked increased asthma rates to cleaning workers, and suggest that preventative measures be put in place when using chemical cleaners – especially for cleaning disinfectant sprays, bleach, and ammonia.
Is it Safe to Use Disinfectant and Cleaning Products While Pregnant?
A large study which was published in 2018 concluded that chemical use while pregnant resulted in an increased risk of the child in utero developing wheezing and/or asthma. These findings were then taken and turned into many different news articles and reports stating that cleaning while pregnant is dangerous for the health of the unborn child, which, really, never was proven. What got missed was the fact that there actually was no significant relationship found between chemical exposure and lung function tests. Another thing to note is that the findings for cleaning product use and asthma symptoms were all self-reported through questionnaires, meaning no asthma cases were ever confirmed with a medical professional.
In response to the misconceptions being reported by the media as a result of this study, the United Kingdom National Health Service (NHS) issued a statement and a review of the paper – ensuring that parents should not be overly concerned with cleaning regimes, so long as they follow general safety protocols by ensuring rooms are adequately ventilated and precautions are taken to protect oneself from touching and inhaling fumes (i.e. gloves and a mask).
While there is currently not a large body of evidence surrounding this topic, calling for a more in depth review to be done, the American Pregnancy Association also ensures that cleaning products, including properly diluted bleach, are safe to use while pregnant. They too recommend wearing gloves, ventilating the room, and reading any labels prior to use. Or, even better, getting the un-pregnant partner to take on the cleaning for a change (*wink wink*).
What are the Safest Cleaning Compounds for Disinfecting?
First of all, there is a difference between cleaning and disinfecting. Cleaning removes germs, dirt and impurities on surfaces and using soap and water can remove germs, not necessarily kill them, to reduce the spread of infection. Disinfecting kills germs on surfaces but doesn’t necessarily remove germs. So while hand washing with soap and water is the best way to clean and get rid of germs but if there is a reason to fear a contaminant has been spread onto a surface of the home, then washing the surface with soap and water, followed by a sanitizer or disinfectant, would be the best course of action.
The Environmental Protection Agency (EPA) has a comprehensive list of disinfectants or sanitizers that are approved to kill viruses like Covid-19 which are generally grouped as:.
- Quaternary ammonium compounds (“quats”) like Lysol heavy duty disinfectant
- Iodine based sanitizers
- Acid anionic sanitizers (peracetic acid)
- Hydrogen peroxide sanitizers like Clorox
- Thymol (a natural and botanically based disinfectant)
- Or Alcohol (ethanol), which you can easily buy in 70% ethanol bottles either wipe items down or transfer it to spray bottles.
Choosing “eco-friendly” alternatives to sanitizers is, of course, an option, as most popular brands now have a “green” alternative for a higher price. I’ll leave a link below to some of the EPA approved “safe” products but an example that I have seen on shelves is some of Seventh Generation products.
Note that homemade products like baking soda and vinegar or lemon juice are fine for cleaning your home, but are not germicides and therefore do not kill any germs well enough to sanitize.
As for those who rely on essential oils as their sanitizer of choice, caution should be taken with this method of cleaning in order to avoid viruses such as COVID-19. While we are starting to see more research surrounding the potential benefits of essential oils for cleaning, it is still lacking. One review found that while some oils have shown antimicrobial properties, their effectiveness relies on the individual oil’s chemical constituents, the quantity of these compounds, as well as the particular properties of the bacteria it is aiming to kill. So, basically, some oils may have an effect on some bacteria, but an individual oil will need to be matched with a specific microbe in order for the disinfectant properties to take place. These studies were also held in vitro within a lab, and have failed to provide any clear mechanism of action – leading the researchers to worry about reproducibility and the accuracy of their findings. The bottom line is that more research is needed, as well as clinical trials, in order to create any clear and scientifically validated recommendations for replacing your household sanitizers with essential oils. This is simply because FDA approved sanitizers kill up to 99.9% of germs, which is something that essential oils cannot yet claim.
What about soap? Can it be used on my counters and high-touch surfaces in place on a chemical disinfectant?
Handwashing, as rudimentary as it may seem, protects us because it has the potential to “inactivate” the virus before effectively washing it down the sink – IF the handwashing is done properly, and for 20 seconds. In the same way soap attaches to the oil and dirt on our hands to wash the debris down the sink, so too does it attach to the molecules that are responsible for infecting us with Coronavirus. Because of this, the most effective, easy, and sensible way to break the chain of infection is with proper, and regular, hand washing. This can be done with any regular soap, as there is no extra benefit of using an antibacterial soap if proper handwashing procedures are followed.
An antibacterial sanitizer or disinfectant is still the #1 recommendation for cleaning high traffic surfaces in your home because they can kill 99% of germs in seconds. BUT, if cleaning supplies are short in your area, soapy water and some elbow grease can still do the trick! Following the same logic as with proper handwashing, surfaces can be scrubbed with soapy water for at least 20 seconds and then thoroughly rinsed in order to ward off germs and virus’.
Using Targeted Hygiene in Covid-19
Global pandemic or not, if we are to maximize our beneficial microbial exposure, while at the same time protecting ourselves from infections and disease, the guidelines around sanitation and hygiene require an update based on the current literature.
The misconception that still roams today that good hygiene and cleanliness are problematic is outdated and needs to be addressed. While we know that being exposed to an array of microbes is important, we also know that not protecting ourselves from harmful pathogens can be detrimental to our health. I am sure this point will be driven home due to the current situation, but the belief that children must be exposed to harmful microbes in order to build a robust immune system is simply not true – this has never been the case. Yet, before the world was launched into a global pandemic, 23% of parents still believed that this myth was true.
So, it is clear that there need to be clearer guidelines on WHAT is okay and safe, and what is not! Targeted hygiene aims to do just that; it is a risk assessment directed at determining the high-risk situations, where pathogenic transmission is more likely, from low-risk situations where microbes are not harmful and/or there is not a high risk of exposure. This allows us to protect ourselves from harmful or infectious microbes, while still retaining the beneficial and/or commensal microbes in our environment.
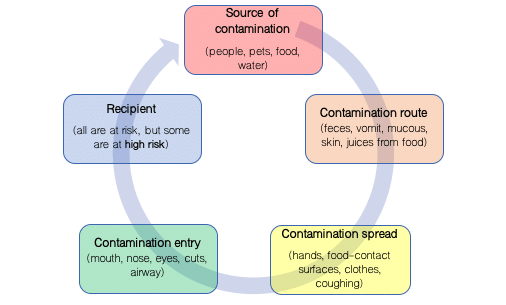
Below, figure 1 outlines “the chain of infection”, a strategy that was designed to be used during the risk assessment portion of targeted hygiene, which was developed by the International Scientific Forum on Home Hygiene (IFH). The chain is supposed to help in the determination of high-risk situations, which then can be treated appropriately to reduce the risk of infection.
When referring to the chain of infection, it is important to remember that there are particular situations where harmful microbes are more likely to be present and/or spread. These are the times that practicing hygiene in order to break the chain of infection is important. These high-risk times include:
- During food handling
- While eating with hands
- After using the washroom
- After coughing or sneezing into hands, or nose-blowing
- After handling soiled or dirty linen
- After handling or disposing of garbage
- Caring for animals
- When caring for an infected family member who is spreading contaminants into the environment through vomiting, coughing, and/or diarrhea.
The Bottom Line on the Role of Disinfectants and Over-Sanitization on our Health and Microbiome
Getting outdoors, socializing with peers, family, and friends (once social distancing is lifted), playing with pets, and the natural environment (aka getting dirty!) are all great ways to gain exposure to a beneficial array of microbes – which help to promote our overall health and immunity. This is especially true at an early age. However, the misnomer that exists that claims there is no need to maintain hygiene and cleanliness in the home, needs to be buried. There is no high-quality evidence supporting the fact that home and personal hygiene is linked to an increased risk of adverse health outcomes – actually, quite the opposite. Failing to comply with basic sanitation protocols, especially after being exposed to a high-risk situation, is increasing the risk of disease and infection. For this reason, targeted hygiene should be practiced in the home, regardless of whether or not there is a global pandemic afoot. Being able to identify risky situations and appropriately respond, while also being able to recognize low-risk or beneficial situations, is key to creating and maintaining a healthy and well-rounded microbiome and immune system.
However, ensuring you are following the instructions on the labels of your cleaners is key – as breathing in and using bare hands to handle chemicals may be linked to several negative health outcomes. Wearing gloves and a mask is necessary, and opening a window in order to allow for airflow should help with the safety of using these cleaners. Also, ensure you are properly diluting your cleaners if the instructions call for this, especially with anything containing bleach. Use the theory of targeted hygiene and consider when the use of disinfectants or “heavy-duty” cleaners is really called for.
SO, do not stress over your seemingly hypervigilant cleaning rituals that have developed. BUT, take the time to recognize which situations are high-risk and which are not, perhaps the excessive cleaning is not called for if there hasn’t been exposure to a potentially risky situation outside, or inside, the home. While interacting with peers is currently off the table with social distancing, still allowing your children to interact with their outdoor environment should be encouraged, as this is a low-risk and beneficial exposure to microbes.
Stay safe!
Contribution by Amber Whittemore
Updated on October 4th, 2021

Abbey Sharp is a Registered Dietitian (RD), regulated by the Ontario College of Dietitians. She is a mom, YouTuber, Blogger, award winning cookbook author, media coach specializing in food and nutrition influencers, and a frequent contributor to national publications like Healthline and on national broadcast TV shows.









Warren Bobinski says
What about the use of Hypochlorous acid – Electrolyzed water as a cleaner? There seems to be a lot of research concerning how safe this is in protecting micro biome, while eliminating virus and germs. It’s good safe and can be made with just salt and water and a proper single cell generator. Our bodies create this naturally, and it’s readily available (salt and water) inexpensive, effective and has several hundred studies proving effectiveness.
It’s been proven effective in hospital sanitation, food services, and has studies regarding cytotoxicity –
Would love to hear what your thought are (I’ve also researched this for the last few years and as. Disclosure have brought a product to market that is consumer friendly and creates hypochlorous acid from salt and water)
Regards,
Warren Bobinski
Egret Canada.
Abbey Sharp says
Thanks for the feedback! I’ll have to look into it.